How Genetics May Affect Ovarian Cancer Risk
-
Updated September 28, 2020
A woman’s risk for ovarian cancer depends on many different factors, from age, to hormones, to environment; but genetics also play a role. So, if a relative was affected—or you have ovarian cancer yourself—you may want to consider undergoing genetic testing.
Experts know that variations in certain genes can increase the risk for ovarian cancer. Around 1 in 100 US women will get ovarian cancer by age 70, but among women with a mutation in the BRCA1 or BRCA2 genes, that number is much higher. Mutations in other genes, including BRIP1, RAD51C, and RAD51D, can also raise ovarian cancer risk.
Genetic testing compares your DNA code to what experts think the DNA code should look like to function normally.
Getting tested can help women better understand their chances for developing ovarian cancer and allow them to take steps to protect their health. And, if they’ve already been diagnosed with ovarian cancer, it may open the door to new treatment options and provide risk information about developing other types of cancer.
Who should get tested?
Genetic factors can increase ovarian cancer risk, but most cases of ovarian cancer aren’t caused by genetics. For that reason, testing is only a valuable option for certain women.
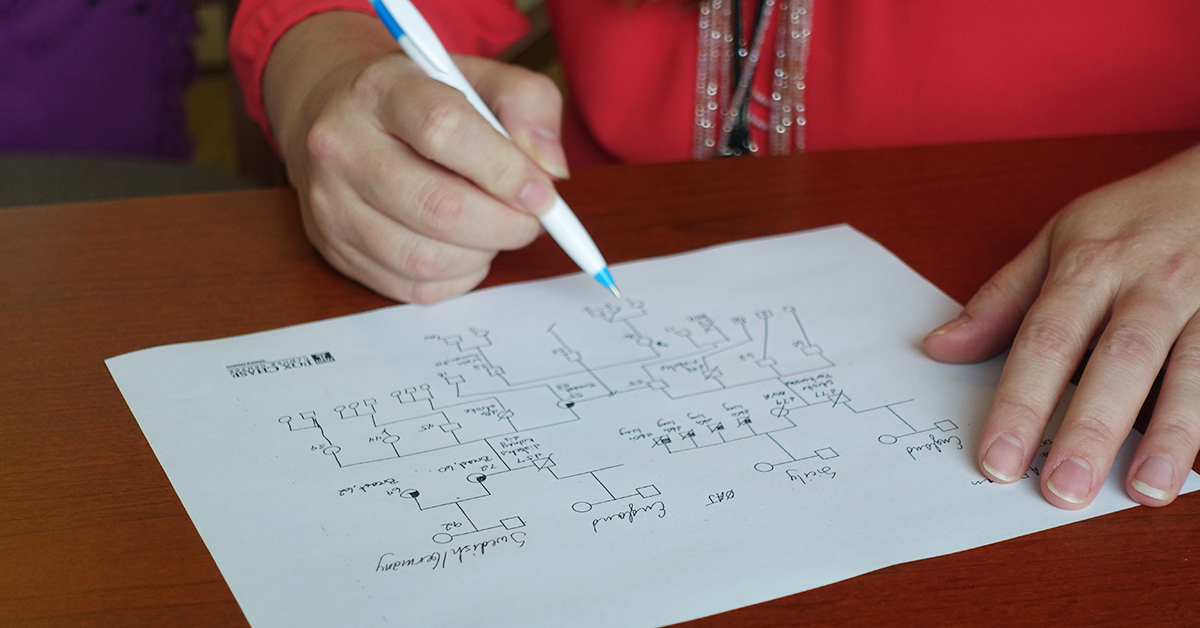
If you haven’t had ovarian cancer, but you have a first- or second-degree relative who has, you should think about testing for yourself. First-degree relatives include a mother or a sister. Second-degree relatives include an aunt or a grandmother.
Testing is also worth considering if you:
- Have had breast, fallopian tube, or peritoneal cancer
- Have been diagnosed or have a close relative who has been diagnosed with breast cancer at age 50 or younger, or a close relative with cancer of the ovary, fallopian tubes, peritoneum, pancreas, or aggressive prostate
- Have a close relative with a BRCA1 or BRCA2 mutation
- Currently have ovarian cancer or you’re a survivor of the disease
A genetic counselor can help you determine whether testing is medically appropriate for you. They’ll also walk you through the pros and cons of testing.
Making the most of your results
Undergoing genetic testing is as simple as giving a blood or saliva sample, but moving forward with your results can be more complicated.
If you test positive for a genetic mutation, you and your doctor can discuss ways to lower your ovarian cancer risk and decide whether you should undergo screening tests for high-risk patients. But remember—having a genetic mutation isn’t a guarantee that you’ll develop ovarian cancer. And, if you already have ovarian cancer, you may now be eligible for chemotherapies targeting BRCA mutations.
Your genetic counselor can also help you share positive test results with family members who may be at risk for having the same mutation.
Are you interested in getting tested?
The Department of Clinical Genetics at Fox Chase offers a Risk Assessment Program for individuals and families at risk for cancer and those with cancer. To make an appointment with one of our clinical genetic specialists, call 877-627-9684.
Reviewed by Fox Chase genetic counselor Catherine Neumann, MS, LCGC
