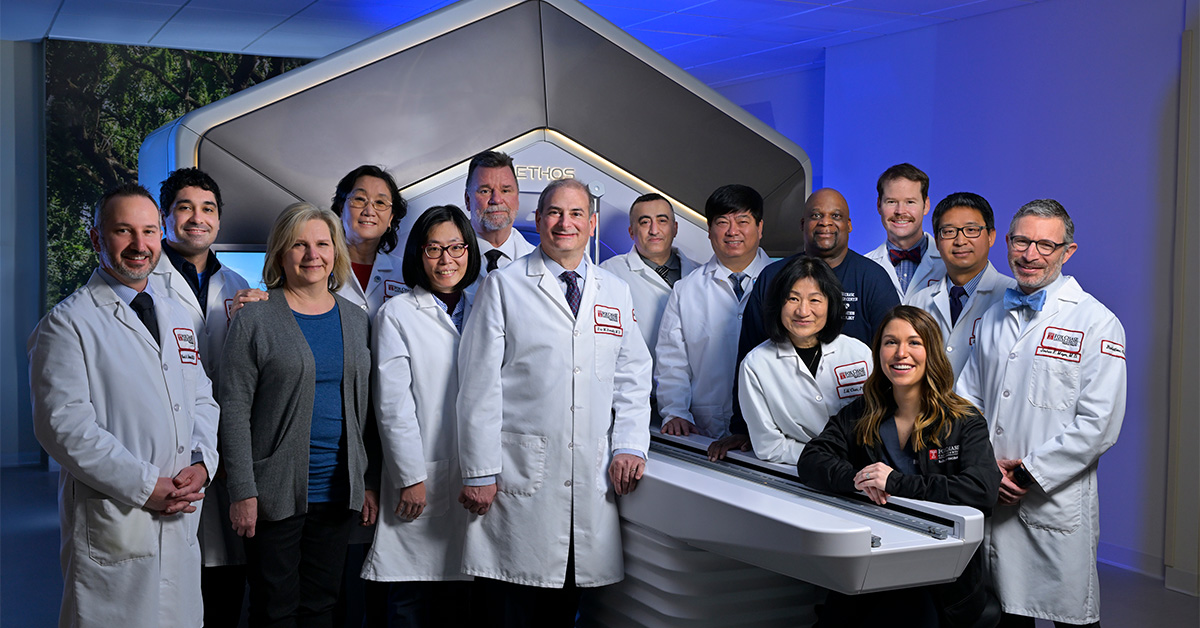
PHILADELPHIA (March 27, 2024) — Over the past year, the Fox Chase Cancer Center Radiation Oncology team led by Eric Horwitz, MD, FABS, FASTRO, Chair of the Department of Radiation Oncology at Fox Chase and the Lewis Katz School of Medicine at Temple University, has boldly moved adaptive radiation therapy into the mainstream, demonstrating its clinical advantages for treating prostate, bladder, liver, pancreas, breast, lung, and head and neck cancers. Horwitz says, “We have built Fox Chase into a national and regional leader offering a robust clinical care program, innovative clinical trials, and the experience of treating many patients.”
At Fox Chase, clinicians and physicists use the Ethos cone-beam computed tomography (CBCT)-based adaptive radiation therapy system of Adaptive Radiation Therapy. This FDA-approved technology combines a linear accelerator that includes CBCT imaging technology and artificial intelligence-based software to power the adaptive treatment process.
The difference between Ethos adaptive radiation therapy and traditional intensity-modulated radiation therapy (IMRT) or stereotactic body radiation therapy (SbRT) is that with non-adaptive IMRT or SbRT, the patient’s unique treatment plan is created just once before the start of treatment. With Ethos, a new treatment plan is made before each fraction of radiation is administered while the patient is on the linac treatment couch.

The new “adapted” treatment plan is based on the size and location of the cancer and the surrounding normal organs. This new plan considers the patient’s response to treatment and the position of all the normal organs and represents the most precise radiation treatment plan possible. The new adapted plan is compared to the pre-treatment plan.
The best plan, defined as superior target coverage or superior normal tissue radiation dose avoidance in one or more adjacent organs at risk, is selected for treatment. This is done for every fraction of radiation. Modifying the daily radiation treatment based upon what is in front of the radiation oncologist ensures that the patient is getting the most accurate and precise treatment possible.
“What we’ve learned as we have gained experience using adaptive radiation therapy is that there is significant daily variation in a patient’s treatment plan, which has surprised us,” says Horwitz, “and this is as true for prostate, bladder, and pancreatic cancer as it is for oligometastatic disease in the spine or abdominal or pelvic lymph nodes.
“The great news is that any candidate for IMRT or especially SbRT may also be eligible for adaptive radiation therapy,” says Horwitz. “As significant as the improved target volume coverage is the absolute reduction in radiation dose to the surrounding normal parts of the body that we see with adaptive radiation therapy.”
The Fox Chase team took years to develop the resources, clinical knowledge, and infrastructure to bring adaptive radiation therapy to patients. “It was a huge learning curve, but we dedicated ourselves to it: Every Fox Chase radiation oncologist is cross-trained to offer adaptive radiation as an option to every eligible cancer patient. Equally skilled is our partner team of PhD physicists who work directly with us at the linear accelerator as part of standard treatment.
“Our clinical trials program is one of the largest in the country for studying adaptive radiation,” said Horwitz. “We were first in the U.S. to offer a prostate cancer clinical trial using adaptive technology. We are now also recruiting patients for our adaptive cervix study as well as our oligometastatic lymph node study. Soon, we’ll recruit for separate adaptive lung and breast cancer trials for later this year.
“Our mission is to develop this incredibly sophisticated FDA-approved technology so that we can utilize its full potential with as many of our patients as possible. We will soon be able to integrate MRI and PET images into the adaptive process where appropriate to make the treatment even more precise.”
Horwitz continues, “Fox Chase is taking a newly established technology and exploring how far we can advance it: to treat a patient’s cancer with as few side effects as possible for the best quality of life. It’s our mission as a National Cancer Institute-designated Comprehensive Cancer Center.”