PHILADELPHIA (October 1, 2020)—Researchers at Fox Chase Cancer Center recently published a commentary examining clinical practices for breast cancer detection using traditional mammography versus digital breast tomosynthesis on baseline and subsequent screenings.
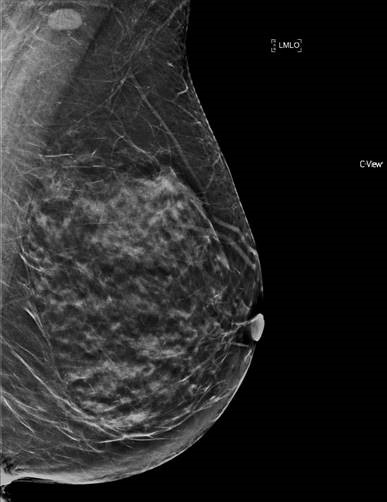
Tomosynthesis is a type of mammography which uses an X-ray imaging technique to take multiple pictures of the breast and construct a 3D-like set of images. It can be used to identify early signs of breast cancer in women with or without early symptoms.
“The take-home point of this publication is that we’re now getting more information about specifically which women benefit from digital breast tomosynthesis over traditional mammography or digital 2D mammography,” said study author Catherine Tuite, MD, associate professor of radiology and section chief for breast radiology in the Department of Diagnostic Imaging at Fox Chase.
According to researchers, mammography remains the standard for breast cancer detection. However, although women who receive breast cancer screenings through mammography have an improved chance of surviving a breast cancer diagnosis, mammograms have limitations such as false positives and high rates of patients coming back for additional screenings.
Tuite said breast tissue density, which can only be determined by a mammogram, is a major factor in the efficacy of mammography. Breast density is categorized as fatty, scattered fibroglandular, heterogeneous, and extremely dense.
She said the more glandular tissue a patient has, the whiter a mammogram appears. In those cases, it’s easier for breast cancer to be hidden in the dense breast tissue and not be visible to a radiologist.
“The tomosynthesis mammogram has been thought to be better for finding abnormalities in dense breast tissue, but previous publications regarding that topic lump heterogeneous and extremely dense categories together and compare them to digital mammography,” said Tuite.
While it’s been shown that all women benefit from tomosynthesis over digital mammogram at baseline screening, this study indicates that results of tomosynthesis in subsequent screenings differ according to individual breast density categories.
“For women with scattered density and heterogeneously dense breasts—the two middle groups—those women benefit from decreased recalls and increased cancer detection with subsequent mammograms using tomosynthesis over a 2D mammogram,” said Tuite.
She added that this new data also found that those women with breast tissue categorized as fatty can benefit from decreased recalls but not necessarily increased cancer detection with tomosynthesis. Additionally, women with extremely dense breast tissue don’t benefit from either decreased recalls or increased cancer detection in subsequent mammograms using tomosynthesis after baseline imaging.
“We’re not quite there yet, but we’re working toward more personalized screening studies for each woman depending on her risk profile. Breast density is an independent risk factor for breast cancer, so now we’re taking that into consideration along with family history, gene mutations, or a host of other factors,” said Tuite.
The study, “Benefits of Digital Breast Tomosynthesis Beyond Baseline Screening,” was published in JAMA Network Open.