Fox Chase pancreatic cancer specialists use advanced surgical techniques whenever possible, including minimally invasive and robotic surgeries for smaller incisions and faster recovery. Our surgical team is fellowship-trained, meaning they have completed up to two years of additional training focused specifically on the highly complex techniques of cancer surgery.
Fox Chase surgeons utilize the latest technologic advances available, and are national leaders in performing complex surgeries for patients with pancreatic cancer. This includes operating on tumors that may be near, or even involving critical blood vessels which need replacement. Our gastrointestinal surgical oncology team works continuously to develop new approaches to treatment and optimize the use of other cancer therapies with surgery.
If your tumor is confined to the pancreas and surrounded by a margin of healthy tissue that can also be removed, upfront surgery may be an option for you. You may undergo radiation and/or chemotherapy before surgery is performed, in order to shrink or downstage tumors that were considered inoperable at one point. Many of our surgical patients undergo a total neoadjuvant therapy (TNT) approach, where a combination of treatments are delivered before surgery, in order to maximize outcomes. Many of our patients enroll in clinical trials, where novel therapeutic drugs, and radiation techniques can be given, in order to treat the tumor before surgical resection. Our surgeons have particular surgical expertise in operating on those who have been treated this way, which may make the procedure more technically demanding.
There are three types of surgery for pancreatic cancer. Your surgery options will depend on where the tumor is located in the pancreas.
Whipple Procedure
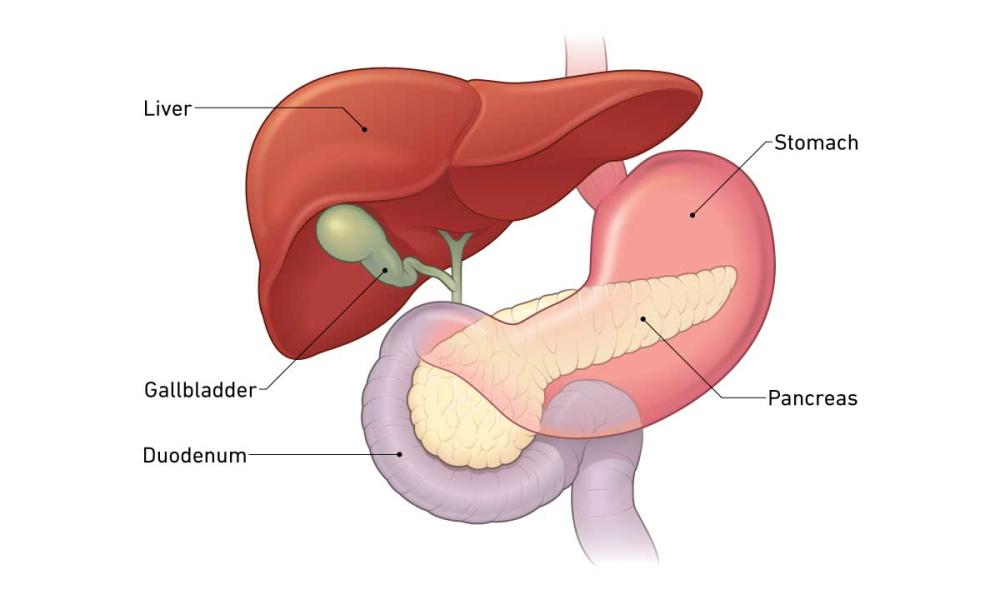
For a tumor in the head of the pancreas (the widest part), the surgery is called a pancreatoduodenectomy—also known as a Whipple procedure. It removes the head of the pancreas, the gallbladder, the duodenum (first part of the small intestine), part of the bile duct, and often part of the stomach. Surgeons also remove nearby lymph nodes to test for cancer cells. There are times where major blood vessels are narrowed by tumors, and removal and reconstruction of these vessels needs to be done. The remaining organs are then reattached to restore continuity of bile drainage, and food digestion. This is the most common surgery for pancreatic cancer.
Distal Pancreatectomy
This surgery removes the body and tail of the pancreas where the tumor is located, along with nearby lymph nodes, and sometimes the spleen and its blood vessels. The spleen helps you battle infections, so your doctor may advise you to get certain vaccines beforehand.
Total Pancreatectomy
This surgery is for cancer of the pancreas that may be multifocal (involving several area of the gland) and removes the entire organ. It also removes the gallbladder, duodenum, part of the bile duct and stomach, nearby lymph nodes, and the spleen. This is done in situations where the disease involves more of the gland or pancreatic duct. When this is being considered, proper preoperative planning with our nutrition and endocrine teams is a key component.
“The multidisciplinary approach is paramount to treating this disease. Our team involves multiple specialists who will step back, look at your case, and become immersed in everything about it. We’ve learned that surgery combined with chemotherapy and/or radiation provides the most optimal results. The best way to do it is to work together, and we do that extremely well.”
– Sanjay Reddy, MD, FACS, Department of Surgical Oncology and co-director of The Marvin and Concetta Greenberg Pancreatic Cancer Institute at Fox Chase